
Guide to Understanding Digestive Health
- 3 Mar, 2025
- 35
What is endoscopy?
Endoscopy is a minimally invasive procedure that examines the inside of the digestive tract using an endoscope, a long, thin, flexible tube with a tiny camera attached at the end.
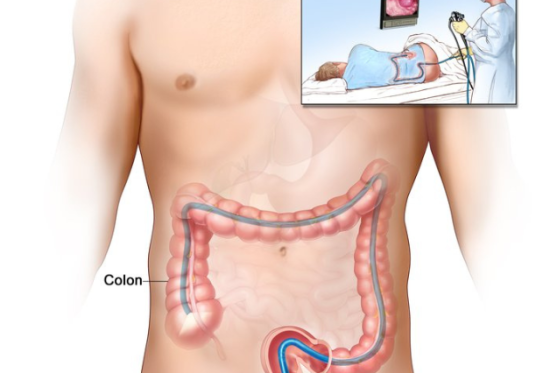
Colonoscopy (known as lower gastrointestinal endoscopy) is a procedure to inspect the inside of the colon (large bowel) using a thin, flexible, tube introduced via the rectum (back passage).
Colonoscopy
What are the indications for a colonoscopy?
Colonoscopy is indicated for investigation of symptoms such as abdominal pain, altered bowel habits, chronic constipation, chronic diarrhoea, rectal bleeding, and weight loss in addition to screening for colorectal cancer and surveillance for polyps and cancer if there is a previous personal history.
How do I prepare for a colonoscopy?
Bowel preparation
You will need to follow a special diet and take bowel preparation medication before your procedure. Printed instructions will be provided at the time of your booking.
The success of your colonoscopy depends on the bowel being as clear as possible, otherwise the examination may need to be postponed, and the preparation repeated.
The bowel preparation induces frequent, loose bowel movements within one to three hours of taking the first dose. It is best to stay at home within easy reach of toilet facilities.
Please notify your specialist if you are pregnant, diabetic, take medications to thin your blood, suffer from disease affecting your kidneys, the heart, or have a pacemaker.
Fasting
After bowel preparation, you will need to stop drinking for approximately two hours before your admission time. The hospital will contact you one working day prior to your procedure to advise on fasting time and admission time.
Medications
You will be given instructions about when to stop your blood-thinning and diabetes medications. Clopidogrel, or similar, Warfarin, Dabigatran or Rivaroxban, NSAIDs, Insulin and oral hypoglycaemics require special instructions.
Please cease iron supplements, anti-diarrhoea drugs seven days prior to the colonoscopy if you are using them:
How is a colonoscopy performed?
Colonoscopy is performed under a light anaesthetic (deep sedation) given by our anaesthetist so that you will be asleep. A sedative medication is given through a vein in your forearm. Once sedated and lying in a comfortable position on your left side, the endoscope is passed through the anus and guided through the colon. Once the endoscope has reached the opening to the small bowel, it is slowly withdrawn, and the lining of the colon is examined again. In some patients, it may not be possible to navigate the endoscope through the full length of the colon—in such cases, further tests may be required.
The entire procedure usually takes between 20 and 40 minutes. Biopsies (small tissue samples) may be taken if abnormal tissue is seen, and polyps (small growths attached to the lining of the bowel) may be removed if necessary. All samples will be sent to a pathologist for examination under a microscope.
Polypectomy
A polyp is an abnormal growth extending from the inner wall of the colon. They vary in size from one millimetre to a few centimetres and can develop into cancer if left untreated. If a polyp is seen during the procedure, it may be removed using special instruments passed through the colonoscope. The tissue is sent to a pathologist for examination under a microscope. Sometimes a polyp may not be removed endoscopically because it is too large or too difficult to reach—in such cases, surgery may be required. Removal of polyps are not painful.
What happens after the colonoscopy?
You must have a relative or friend accompany you home and remain with you for the rest of the day. You cannot go home unaccompanied by public transport or in a taxi. Your procedure may be cancelled if you do not have these arrangements in place.
Following the colonoscopy, you will remain in the hospital recovery area for approximately one up to three hours until the effect of the medication wears off. You may experience slight discomfort or bloating due to the air inserted during the procedure which usually eases with the passage of wind.
If you have a biopsy or polyp removed, you may notice a small amount of blood passed in the toilet. If you develop severe or persistent abdominal pain, bleeding from the back passage, or any other symptoms of concern, you should contact your doctor or go to the nearest hospital Emergency Department.
Because the sedation given may interfere with your judgement or ability to concentrate, you should not drive a motor vehicle, travel on public transport alone, operate dangerous machinery or sign important documents for the remainder of the day.
Our specialist will inform you of your test results on the day of the procedure. A follow-up appointment may be scheduled to discuss the test results more fully. The results of any biopsies or polyps removed typically take one week.
What are potential complications of colonoscopy?
Any medical procedure carries some risk, but colonoscopy is generally considered a safe procedure, and complications are rare. Other complications may exist that are not listed.
Potential complications may include:
Although rare, some of these complications can be serious and may require hospital admission, blood transfusion, further procedures or even urgent surgery. If you wish to have a more detailed discussion about potential risks, please discuss with your specialist prior to the procedure.
What are the limitations of colonoscopy?
While colonoscopy is the best and the most accurate assessment of the colon test for excluding bowel polyps or cancer, however no perfect test and a small proportion of polyps or even cancers may escape detection. In about 5% of patients, lesions can be missed. This may be due to variations in the structure of the bowel, pathology within the bowel or because of inadequate bowel preparation. If this occurs your colonoscopy may need to be repeated another time, or you may need another method of investigation.
Our team perform gastroscopy and colonoscopy at Brisbane Waters Private Hospital and Gosford Specialist Day Hospital on the Central Coast.